UnitedHealthcare Appoints New CEO Following Murder
Leaked talking points detail insurer's PR push amid incoming CEO
UnitedHealthcare named a new CEO on Thursday, a corporation insider who advocated for the use of algorithmic software in health insurance coverage decisions, a practice that relies on computers and so-called “artificial intelligence” to rapidly spit out denials. The appointment comes a month after the murder of previous CEO Brian Thompson by alleged gunman Luigi Mangione.
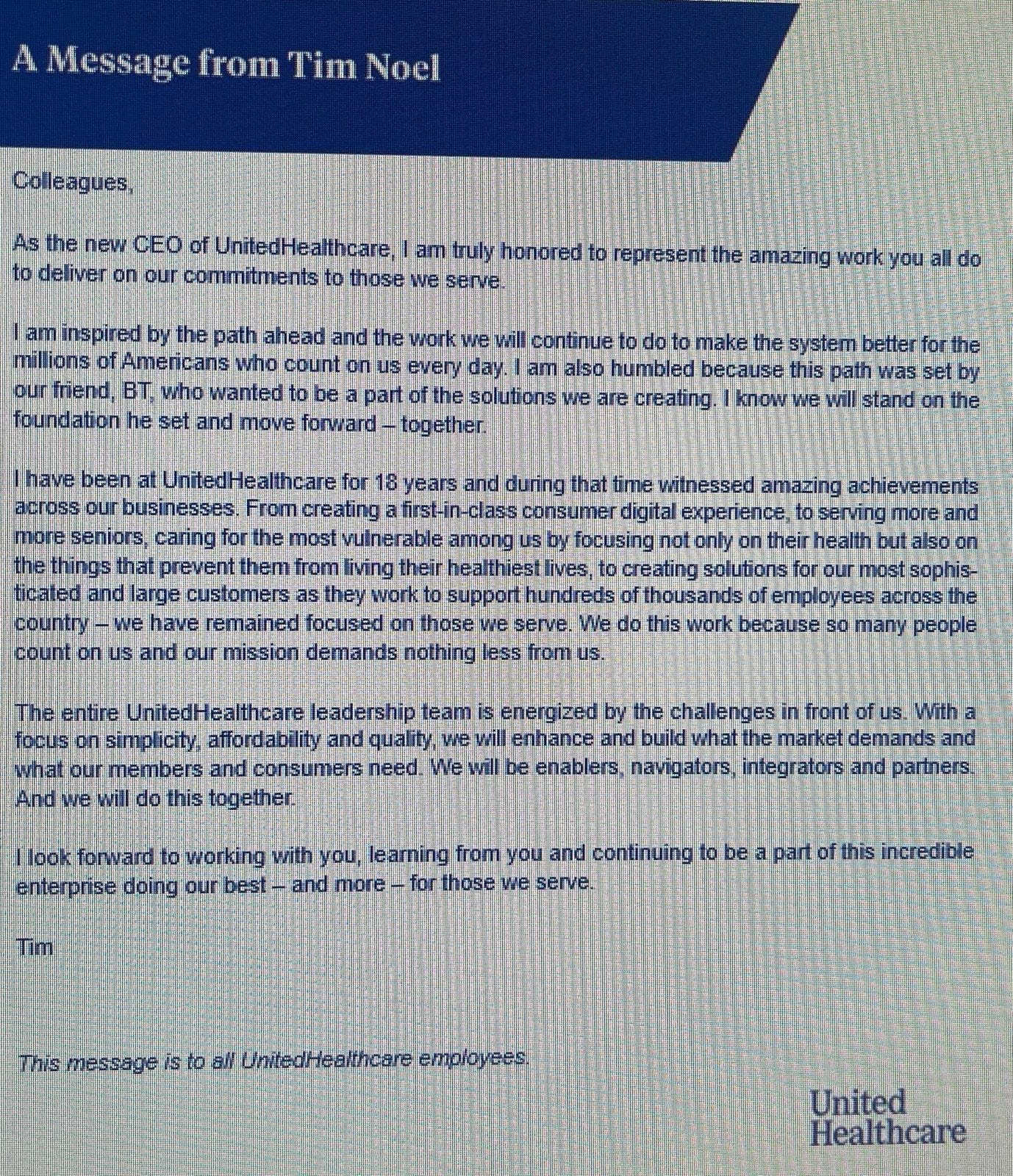
New CEO Tim Noel stressed in a message to staff that there would be continuity with the previous CEO. “I am also humbled because this path was set by our friend, BT [Brian Thompson], who wanted to be a part of the solutions we are creating,” Noel wrote. “I know we will stand on the foundation he set and move forward — together.”
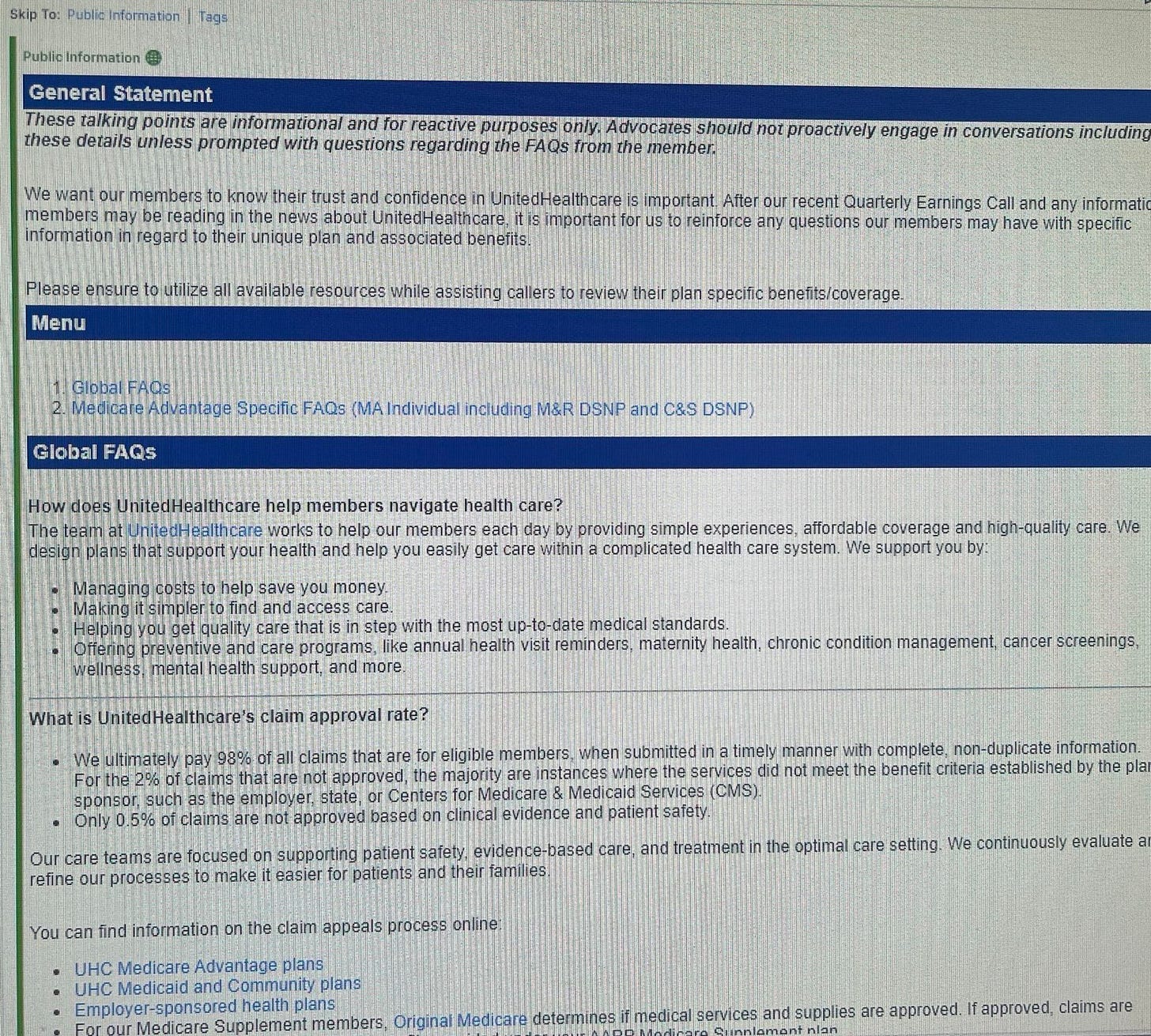
Internal UnitedHealthcare talking points we also obtained focus on the same issues for which the health insurer has faced criticism: claim denials, prior authorization requirements, and the use of artificial intelligence.
A company man, Noel has worked at UnitedHealthcare since 2008, most recently as its head of Medicare and retirement operations. In addition to being the country’s largest health insurer, UnitedHealthcare is also the top provider of Medicare Advantage plans. As head of the division that oversaw Medicare, Noel reportedly fought the federal government’s attempts to rein in companies’ use of algorithms in Medicare coverage decisions.
Noel called the use of algorithmic technology necessary “to ensure access to high-quality safe care and maintain high member satisfaction while appropriately managing costs,” according to a 2023 letter he wrote to the Centers for Medicare and Medicaid Services. The letter appears in a public comment for a new rule being considered by the agency to curb the use of algorithms.
Noel claimed that limiting such “utilization management tools would markedly deviate from Congress’ intent in creating Medicare managed care because they substantially limit MA [Medicare Advantage] plans’ ability to actually manage care.”
In 2024, the federal government Centers for Medicare and Medicaid significantly narrowed the use of algorithms and AI to determine coverage for elderly patients enrolled in Medicare Advantage. A class action lawsuit is wending its way through the courts on behalf of UnitedHealthcare patients who allege they have been harmed by the company’s algorithmic decision-making. (The company denies the allegations.)
An investigation by StatNews last year alleges UnitedHealthcare wrongfully denied care using algorithms. Per the investigation:
“payment denials were based on an algorithm’s predictions, unbeknownst to patients, and UnitedHealth’s employees were advised not to stray from those calculations — forcing extremely sick and injured patients to pay for care out of their own pockets or return home even if they couldn’t walk or go to the bathroom independently.”
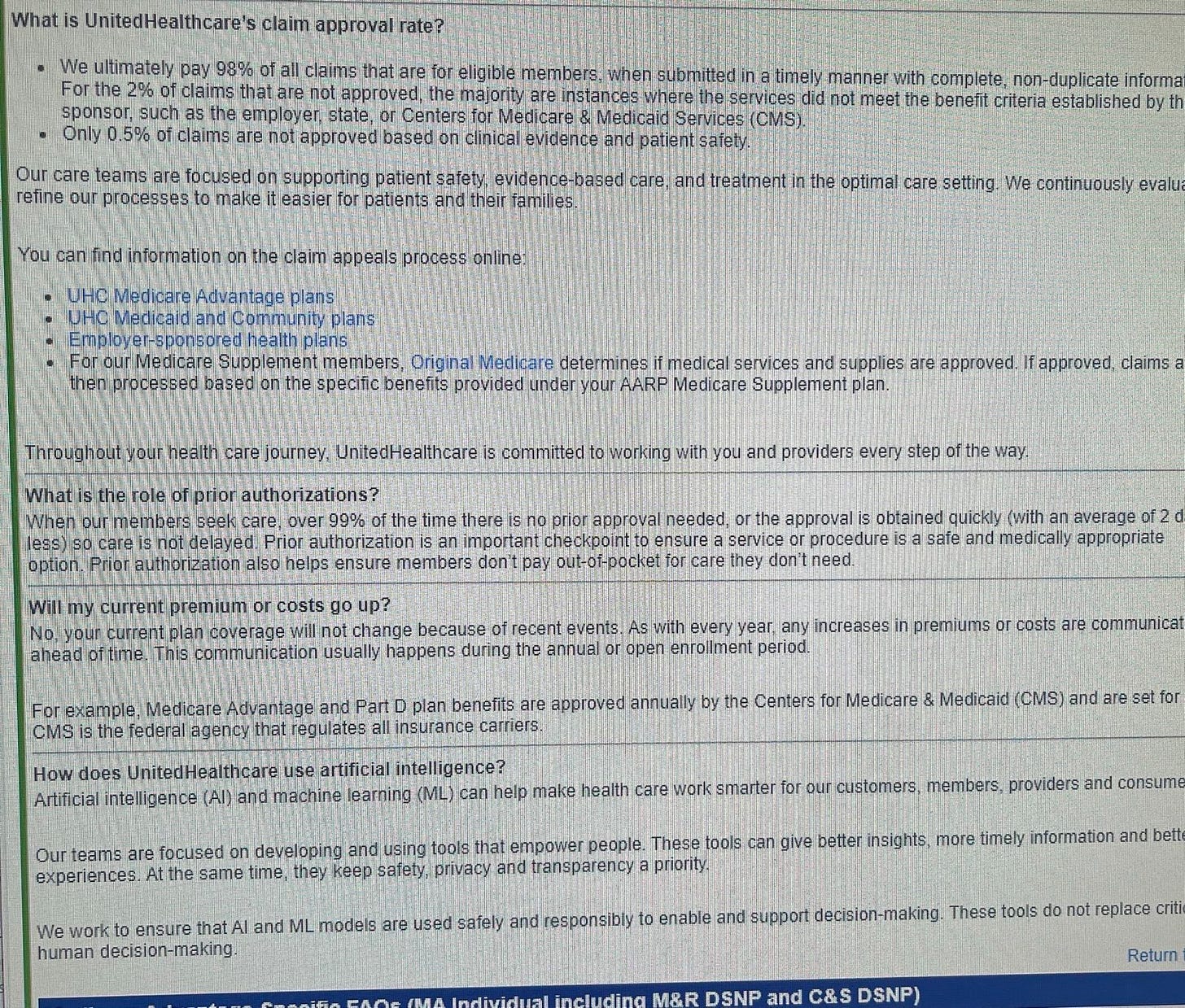
In contrast, UnitedHealthcare’s talking points assert that they cover the vast majority of claims and that their AI tools “do not replace critical human decision-making.” Per the talking points (published in full at the bottom of this article):
“We ultimately pay 98% of all claims that are for eligible members, when submitted in a timely manner with complete, non-duplicate information.”
“For the 2% of claims that are not approved, the majority are instances where the services did not meet the benefit criteria established by the sponsor, such as the employer, state, or Centers for Medicare & Medicaid Services (CMS).”
“Only 0.5% of claims are not approved based on clinical evidence and patient safety.”
“We work to ensure that AI and ML [machine learning] models are used safely and responsibly to enable and support decision-making. These tools do not replace critical human decision-making.”
While there is vanishingly little information about Tim Noel on UnitedHealth’s website, public records we obtained show that his wife was appointed in 2023 as an Assistant Attorney General in Minneapolis where she works on healthcare related issues under state Attorney General Keith Ellison, who sued the company in 2022 to block UnitedHealth’s acquisition of Change Healthcare.
Meanwhile, court records show that in 2019 Tim Noel, his wife Sara, and their home remodeler J.D. Nicholson were engaged in a protracted legal battle with River City Tile over the cost of a kitchen and bathroom renovation estimated at tens of thousands of dollars. A key point of dispute was the cost and production of a “versailles” tile pattern. The suit was settled out of court in 2020.
UnitedHealthcare did not respond to a request for comment.
— Edited by William M. Arkin



Surprise, surprise, they learned nothing from Thompson’s murder.
“We ultimately pay 98% of all claims that are for eligible members, when submitted in a timely manner with complete, non-duplicate information.”
Only after many of them appeal a denial. Which most people haven’t the time or energy to do.
Or in a “timely” manner.
Or without any errors.
In other words, that’s 98% of a much smaller subtotal.